
News Addiction: Global Stress Loops You Don’t Notice

There’s a particular kind of exhaustion that doesn’t come from having “too little empathy,” but from having your care stretched across more suffering than a human nervous system can complete. When pain is delivered in an endless feed—war, disaster, injustice, loss—your system receives an ongoing signal to orient, respond, and resolve. But resolution never arrives.
In that gap, many people notice a confusing shift: numbness, irritability, withdrawal, or a guilty sense of “What’s wrong with me?” This is often labeled compassion fatigue—yet it’s less a character issue and more a capacity issue: a regulatory response to sustained exposure without a pathway to meaningful completion.
What if your shutdown isn’t a moral failure—but your system trying to prevent collapse?
Compassion fatigue is commonly described as emotional and physical depletion that can follow prolonged exposure to others’ suffering. In a globally connected world, that “exposure” doesn’t require being on the front lines; it can arrive through notifications, headlines, livestreams, and images that bypass your usual pacing. [Ref-1]
The experience often has a specific texture: you still care in principle, but your body stops cooperating. Attention skitters away from painful stories. A familiar ache becomes flatness. You might feel guilty for scrolling past, then resentful for being asked (implicitly or explicitly) to keep caring at full volume.
It can feel like you’re failing at compassion, when you’re actually running out of room to hold what you’ve been carrying.
Humans are built to register distress in others as a signal. That signal mobilizes attention, arousal, and social orientation—“Something is happening; do I need to respond?” When those cues keep coming without a “done” signal, the system doesn’t stay gently open forever. It shifts strategy.
One common strategy is protective shutdown: dulling, emotional distance, or a reduced ability to feel moved. This isn’t the absence of care; it’s a load-management response. In discussions of global compassion fatigue, researchers have highlighted how continuous exposure to widespread suffering can strain coping resources, leading to emotional exhaustion and disengagement. [Ref-2]
In other words: when empathy can’t complete into effective response, the nervous system looks for a way to reduce input.
For most of human history, care happened in small groups, at close range, with clearer arcs: a person got hurt, the group responded, the danger passed, the body settled. That cycle offered closure—proof that care led somewhere.
Modern global awareness disrupts that cycle. Your nervous system may receive cues of suffering from thousands of miles away, across many communities, all at once. The signal still lands as “real,” but the response pathway is faint or absent. Over time, this mismatch—high input, low completion—can make caring feel unsustainable. [Ref-3]
This is not a deficit in you. It’s a scale problem: a finite organism living in an infinite feed.
When distress cues are constant, emotional distance can function like a temporary circuit breaker. It lowers arousal enough for you to work, parent, eat, sleep, and keep daily life intact. In that sense, distancing can be a form of self-protection rather than indifference.
In digital environments, especially, the mind can learn to “zoom out,” scroll faster, avoid images, or keep everything intellectual. This can reduce immediate overwhelm, but it also reduces the likelihood of natural closure—because closure depends on experiences being metabolized into something complete, not just avoided or endured. [Ref-4]
When the world keeps arriving as an emergency, where does your system get permission to stand down?
Many people carry an unspoken equation: constant awareness equals moral responsibility. In this frame, stepping back from the news can feel like betrayal—of victims, of values, of one’s own identity as a “good person.”
But constant exposure doesn’t automatically create effective care. In fact, when the nervous system is saturated, the quality of concern can erode: care becomes brittle, reactive, or performative; grief becomes chronic activation; outrage becomes a substitute for agency. Some compassion fatigue resources emphasize that staying compassionate requires avoiding emotional overload—not because suffering isn’t real, but because overwhelmed systems can’t sustain genuine care. [Ref-5]
This is one of the cruel paradoxes of modern awareness: the attempt to prove goodness through nonstop witnessing can steadily reduce the very capacity that makes goodness possible.
Under persistent overload, many people slide into a predictable loop. The system encounters distress cues, mobilizes briefly, then hits the wall of “I can’t do anything,” and seeks relief through distance. Relief arrives—temporarily—so the brain learns that disengagement works.
This loop isn’t driven by a simple emotion like fear. It’s structural: repeated high-intensity input without completion trains the nervous system to bypass contact. Over time, shutdown becomes the default response, not because you don’t care, but because caring has repeatedly led to unresolved activation. [Ref-6]
In Meaning Density terms, the loop tightens when experiences cannot integrate into identity through completed action or resolved connection—so the system chooses the only available closure: disconnection.
Compassion fatigue isn’t one feeling; it’s a cluster of regulatory shifts that help the system manage input. In media-heavy environments, empathy fatigue can show up as reduced emotional responsiveness, irritability, and withdrawal. [Ref-7]
Numbness or flatness when reading painful stories
Cynicism, sarcasm, or a quick turn to judgment
Avoiding news entirely, then feeling guilty about avoidance
Doom-scrolling that feels compelled rather than chosen
Difficulty feeling tenderness in everyday relationships
These patterns are not identities. They are often what capacity looks like when it’s been overdrawn.
One cost of chronic overload is moral fog. When everything is urgent, discernment collapses. You may find it harder to sense what you actually stand for, because your system is busy managing signal volume rather than forming coherent meaning.
Another cost is the quiet thinning of local care. Not because global issues matter more or less, but because the nervous system has limited bandwidth for attunement. Compassion research often notes “compassion fade”: as the number of people in need grows, felt concern can diminish—an effect tied to human limits rather than moral intent. [Ref-8]
In practical terms, this can feel like losing access to your own values. The heart is still there; the channel is overloaded.
When global distress keeps arriving without a realistic pathway to completion, the system learns a bleak association: attention equals pain without resolution. Then, even small cues—an alert, a headline, a friend’s mention of the news—can trigger pre-emptive exhaustion.
This is how a person can become both hyper-aware and emotionally absent at the same time: consuming information while feeling progressively less able to care. It’s a paradox sometimes described as collapsing compassion—where increased exposure doesn’t deepen concern, but instead drains it. [Ref-9]
Withdrawal, then, isn’t just “checking out.” It can be the nervous system’s attempt to prevent continuous, unsatisfied mobilization.
One of the most stabilizing reframes is separating two things that often get fused: caring and constant intake. Caring is a relational orientation; intake is just exposure. When exposure exceeds capacity, the system may reduce intake to protect the ability to care at all.
This is not about “thinking differently” as a quick fix. It’s about the body’s accounting: how much activation arrives, how much resolution is possible, and whether your system ever receives a credible signal of completion. Resources on compassion fatigue often emphasize sustaining compassion by preventing overload—protecting the conditions that allow concern to remain humane and durable. [Ref-10]
Sometimes the most faithful form of care is the one your nervous system can actually carry.
Human systems stabilize when care can move through a full cycle: notice → respond → witness impact → settle. Reachable relationships—family, friends, neighbors, community roles—are more likely to provide that sequence. Not because distant lives matter less, but because completion is more available nearby.
There’s also a known phenomenon sometimes called “psychic numbing”: as suffering becomes large-scale and statistical, the mind can struggle to feel proportionate concern. [Ref-11] This isn’t coldness; it’s the brain protecting itself from unfinishable magnitude.
When care returns to contexts where response is tangible, coherence often returns with it: values become clearer, identity feels less fractured, and concern stops being a flood and becomes a channel.
As load reduces and experiences become more completable, many people notice a different quality in their attention. The body is less braced. The mind can stay with a difficult story without either spiraling or going blank. This is not about becoming endlessly sensitive; it’s about recovering capacity for signal return.
Burnout research often describes depletion as involving emotional exhaustion and reduced efficacy; as those pressures ease, people often report renewed effectiveness and steadier engagement. [Ref-12] In compassion fatigue, a similar shift can appear: less urgency, more discernment; less performative outrage, more grounded concern.
Not “more feeling,” but more steadiness: the sense that you can care without losing yourself.
Compassion is often described not as absorbing others’ pain, but as a response that includes the wish to reduce suffering. [Ref-13] When compassion fatigue lifts, care tends to become more directed—less diffuse scanning, more specific orientation. The nervous system can distinguish between what is tragic and what is actionable, without denying either.
In Meaning Density terms, directed compassion increases coherence because it links values to lived identity through completed loops: a response that reaches an endpoint, a contribution that lands, a relationship that holds. That completion is what allows the system to stand down and return to baseline.
Global awareness can still exist—but it no longer has to function as a constant alarm. It can become information you can metabolize, rather than a perpetual emergency you must carry.
Compassion fatigue often appears when the world asks your nervous system to do something impossible: remain continuously open to suffering without a pathway to meaningful completion. In that context, numbness and withdrawal are not evidence of being “uncaring”—they are evidence of a system protecting its remaining capacity.
When care is aligned with what can be held, finished, and integrated into a life—when it has some form of closure—agency tends to return. Not as pressure, but as orientation: a sense of where you actually are, what you actually value, and what your system can genuinely support. Clinical and wellness discussions of compassion fatigue often frame it as a cue to restore balance between caring and capacity. [Ref-14]
You don’t preserve compassion by knowing everything, witnessing everything, or staying perpetually activated. You preserve it when your care remains connected to a human scale—where concern can become a real response and then come to rest.
In a world that monetizes your attention and treats your alarm as proof of goodness, it is quietly radical to let compassion be sustainable. Not smaller—truer. [Ref-15]
From theory to practice — meaning forms when insight meets action.
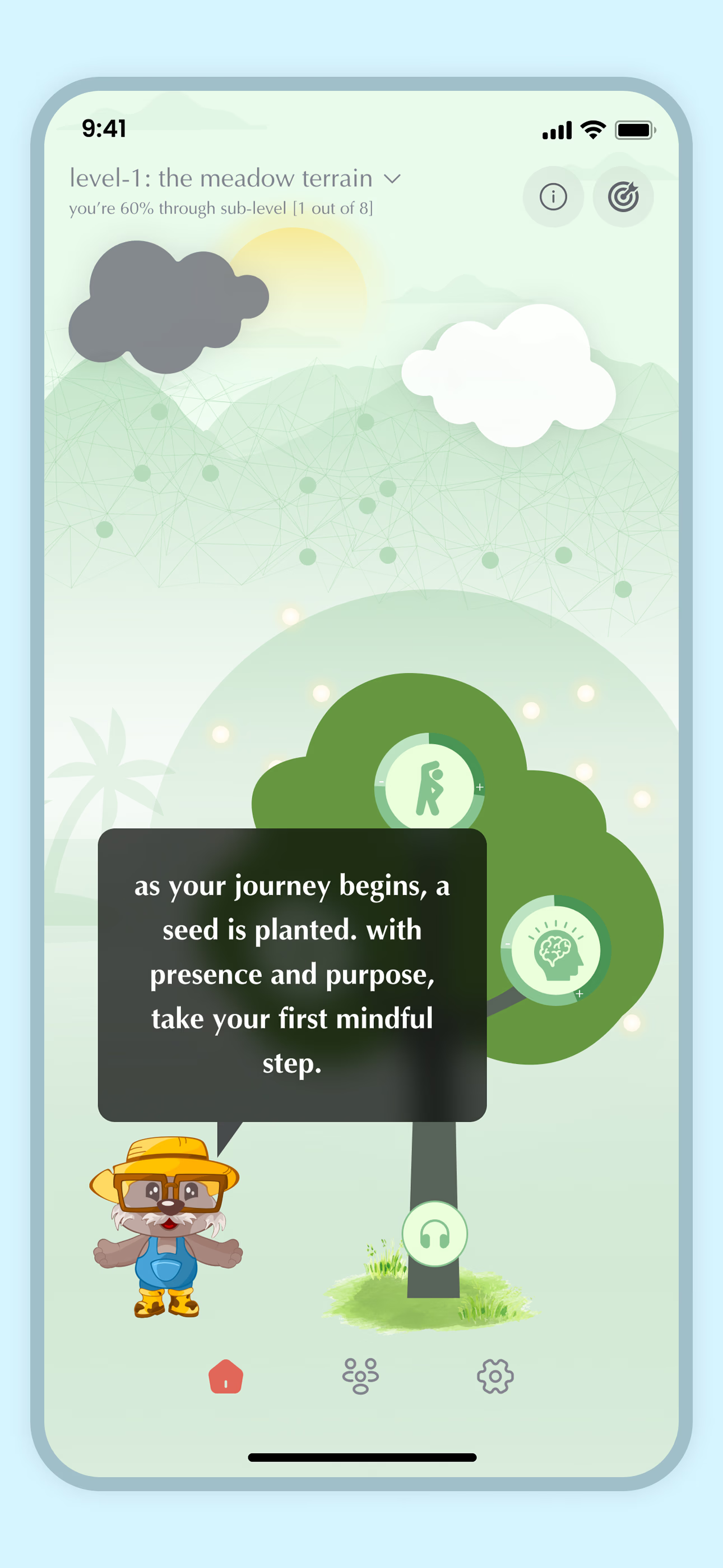
From Science to Art.
Understanding explains what is happening. Art allows you to feel it—without fixing, judging, or naming. Pause here. Let the images work quietly. Sometimes meaning settles before words do.