
Resetting After Emotional Shock: Nervous System Recovery

Emotional recovery time is the period your nervous system needs to recalibrate after intensity—conflict, disappointment, uncertainty, change, grief, pressure, or even sustained “being on.” It’s not the same as understanding what happened, or being able to explain it well. It’s the slower return of your body’s internal settings: breath, sleep depth, muscle tone, attention, appetite, and the sense that things are no longer urgent.
Why am I still not back to normal if the situation is already over?
In modern life, many people expect recovery to be quick because the calendar moves on quickly. But biology doesn’t run on deadlines. When recovery takes longer than seems reasonable, that gap often gets interpreted as personal weakness. More often, it’s simply incomplete closure: the system hasn’t received enough safety cues, completion signals, or uninterrupted downshift time to stand down.
A common frustration is the mismatch between what you think you should be able to do and what your body can currently support. You show up to work, respond to messages, make meals, and look “fine,” yet a part of you stays wired, heavy, or brittle. That can spark a second layer of stress: self-criticism, impatience, and the feeling that you’re falling behind.
It’s worth naming that self-judgment often arrives when the nervous system is already carrying load. Under stress, the brain becomes more threat-focused and less flexible, which can make inner commentary feel harsher and more absolute than it would otherwise. [Ref-1]
Sometimes the hardest part isn’t what happened—it’s how quickly you’re expected to be over it.
After emotional stress, multiple systems have to settle: stress hormones shift, the autonomic nervous system adjusts, and the brain updates its predictions about safety and what to expect next. This doesn’t resolve at the speed of a decision. It resolves at the speed of physiology.
Even when you can accurately label what you felt and why, the body may still be running a protective program—elevated alertness, shallow rest, or heightened startle—because it hasn’t completed the full cycle back to baseline. Stress-related changes in arousal and threat detection can persist beyond the triggering event, especially when the event involved uncertainty or social evaluation. [Ref-2]
Understanding can be fast. Settling is slower.
From an evolutionary standpoint, it would be risky to “snap back” instantly after a threat. A system that stands down too quickly could miss danger signals and pay a high cost. So the body is designed to resolve stress thoroughly—checking the environment, re-establishing safety, and restoring internal reserves.
This is part of what researchers describe as allostasis: the body’s process of maintaining stability through change. When stress is frequent or prolonged, the “wear and tear” of maintaining readiness accumulates, and recovery tends to require longer windows for recalibration. [Ref-3]
In other words, needing more time isn’t a character flaw. It can be a sign that your system is doing what it was built to do: not just react, but ensure resolution.
Many people can override activation temporarily. You can socialize, perform, problem-solve, and keep moving—sometimes impressively. But forcing a quick recovery often changes the outward appearance more than the internal state.
When the body doesn’t get enough closure, activation can stay running in the background: tighter sleep, more irritability, more scanning for problems, less tolerance for ambiguity. The system may look functional while still paying a physiological cost. Over time, chronic stress patterns can shift baseline functioning and make downshifting less available on demand. [Ref-4]
What looks like “bouncing back” can sometimes be “continuing while activated.” Those are not the same process.
Modern culture often treats recovery like a luxury—something you earn after you’ve proven you’re fine. There’s an unspoken standard that a capable person should be quick, upbeat, and efficient again. But the nervous system doesn’t interpret social expectations as safety cues.
Systems recover through sufficient time, reduced demand, and signals of safety—not through being told to “be resilient.” When those conditions are missing, stress load can accumulate in ways that correlate with burnout symptoms and reduced capacity. [Ref-5]
Insufficient emotional recovery doesn’t just leave you tired. It changes what happens next. When the body remains partially activated, everyday stressors land harder. Small conflicts feel bigger. Minor decisions feel heavier. The threshold for overwhelm drops.
This is how a loop forms: stress happens, the system doesn’t fully recalibrate, and then the next stressor arrives on top of remaining activation. Over time, this compounding load is associated with burnout-related patterns and broader health strain. [Ref-6]
Importantly, this isn’t about “not coping well enough.” It’s about the structural math of nervous system load plus insufficient completion signals.
People often expect recovery problems to look like extreme distress. But under-recovery can be quiet and subtle—more like a reduction in bandwidth than a visible crisis.
After acute stress, it’s common to notice lingering aftereffects as the system stabilizes: changes in sleep, attention, irritability, sensitivity, or fatigue. [Ref-7]
These aren’t identities. They’re regulatory responses—ways the nervous system attempts to manage incomplete downshift and muted closure.
Recovery is where resilience is built—not by adding more effort, but by restoring capacity. When recovery stays incomplete for long stretches, the system can begin to feel fragile: less buffer, less tolerance, less ability to return to baseline after ordinary strain.
Chronic under-recovery is closely tied to burnout patterns: emotional exhaustion, reduced efficacy, and a sense that even small tasks carry disproportionate weight. [Ref-8]
It’s not that you can’t handle life. It’s that life has been arriving faster than your system can finish its cycles.
One of the most confusing experiences is noticing that recovery seems to take longer now than it used to. This can happen when the body’s baseline activation shifts upward after repeated stress without enough stand-down. The system becomes quicker to mobilize and slower to fully settle—less because of “sensitivity,” more because the set point has been nudged by repeated demand.
Sleep is a key part of this recalibration. When sleep is disrupted by stress—and stress is worsened by poor sleep—the cycle can reinforce itself, making recovery windows feel even more expensive and harder to access. [Ref-9]
In that context, “needing more time” is not regression. It can be the honest time-cost of returning to baseline when baseline has been strained.
It can help to distinguish three different experiences: relief, stimulation, and restoration. Relief reduces discomfort in the moment. Stimulation changes state quickly. Restoration is slower: it’s the nervous system re-establishing rhythm, letting signals complete, and receiving enough safety cues that it can stop scanning and stand down.
This is why “doing something fun” doesn’t always equal recovery. Enjoyment can be real, but the deeper recalibration depends on autonomic shifts that take time and require fewer interruptions. Research on chronic stress and the autonomic nervous system describes how recovery involves gradual rebalancing, not instant resets. [Ref-10]
Recovery isn’t a performance. It’s a biological completion.
Because stress is deeply social, recovery is also shaped by social context. When people around you minimize what happened, rush you, or subtly evaluate your timeline, your system may stay in “prove you’re okay” mode—an ongoing activation that delays stand-down.
On the other hand, when your experience is met with patience and ordinary respect, the nervous system often has an easier time recalibrating. This isn’t about being coddled; it’s about receiving cues that the environment is stable enough for recovery to complete. Practices that involve nonjudgmental attention and reduced internal pressure are associated with changes in body-based regulation pathways. [Ref-11]
Being believed and not rushed can be a safety cue all by itself.
Restored capacity is often more ordinary than people expect. It’s not necessarily euphoria or high confidence. It’s the quiet return of range: you can think, choose, and respond without needing to brace first.
Many people notice signs like these as the system settles:
Supportive connection can function as a buffer for stress physiology, helping the system find baseline again. [Ref-12]
When you allow recovery to complete, something subtle but important can return: trust. Not a motivational kind of trust, but a body-level trust that your signals matter and your limits are not emergencies. That trust reduces internal conflict, which reduces load.
Over time, honoring recovery also protects meaning. When life is lived in constant override, identity can narrow into roles—producer, caretaker, fixer, achiever—while the felt sense of self becomes harder to access. Adequate recovery time helps experiences land, resolve, and integrate into a coherent narrative instead of remaining as ongoing activation.
Social disconnection and perceived isolation can intensify stress load, while reliable connection supports regulation and health—another reminder that recovery is not only individual willpower. [Ref-13]
In a world that treats speed as virtue, emotional recovery time can look like falling behind. But biologically, it’s an investment in long-term coherence: the ability to live from values instead of urgency, to respond instead of react, to carry fewer unfinished loops into tomorrow.
When you relate to your recovery needs with less criticism, you reduce one of the most common sources of extra load: the pressure to be different than your nervous system currently can be. Research on self-compassion suggests that lowering self-criticism is associated with better psychological outcomes, in part because it changes the internal threat climate. [Ref-14]
Recovery doesn’t mean your life is smaller. It often means your life becomes more livable—because your system can finally register “enough,” “safe,” and “done.”
Emotional recovery is not a detour from living. It’s the process that lets living feel real again—less fragmented, less forced, more internally aligned. When recovery is allowed to complete, the nervous system spends less time bracing and more time participating.
Over the long run, that completion protects your capacity to care, connect, and choose with integrity—because your body isn’t constantly paying the hidden costs of unfinished activation. The steadier life isn’t the one with the most intensity managed; it’s the one with enough closure to let the system stand down. [Ref-15]
From theory to practice — meaning forms when insight meets action.
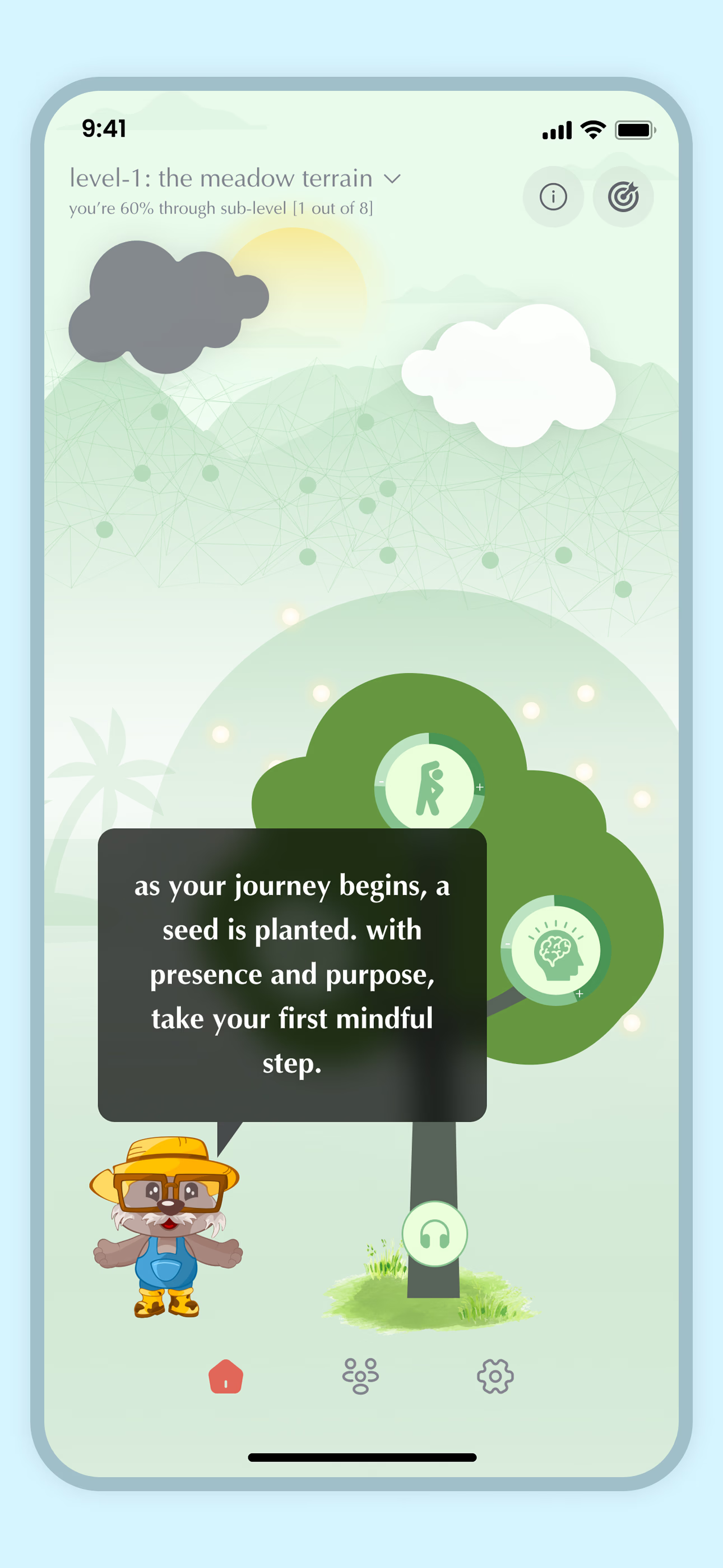
From Science to Art.
Understanding explains what is happening. Art allows you to feel it—without fixing, judging, or naming. Pause here. Let the images work quietly. Sometimes meaning settles before words do.