
Stress Accumulation: How Daily Micro-Stress Builds Into Burnout

There are days when you can carry a lot: the schedule changes, the noise, the decisions, the small disappointments. Then there are days when one extra email, one misplaced item, or one slightly tense conversation seems to tip everything over.
Why does the same life feel manageable on Monday—and impossible on Thursday?
“Stress threshold” is a helpful way to name this. It’s the variable point where accumulated load meets reduced capacity, and your system shifts from regulation into reactivity or collapse. That shift can look emotional, physical, social, or cognitive—but underneath, it often reflects a body doing its best to protect what resources it has left.
People often describe it as being “fine” and then suddenly not fine. A minor inconvenience lands like an attack. A neutral comment feels sharp. A normal request feels impossible. From the inside, it can seem abrupt and confusing—like your reaction arrived without a runway.
But nervous systems don’t usually flip states because of a single moment. More often, the “small thing” is simply the first thing that arrives after your internal buffer has thinned. What looks like a disproportionate response is frequently a proportional response to total load, not the final trigger. [Ref-1]
Sometimes the breaking point isn’t the last drop—it’s the invisible accumulation.
Your stress threshold rises and falls with the basic variables that govern capacity: sleep quality, physical recovery, nutrition and hydration, cognitive demand, social strain, ongoing uncertainty, pain, hormonal shifts, and the constant “holding” of unfinished responsibilities.
Even when each factor is small, they stack. Micro-stressors accumulate in the background: deciding, tracking, switching, responding, anticipating. If recovery is partial, the system carries forward yesterday’s residue into today, and the threshold gets lower without any dramatic event announcing it. [Ref-2]
When load stays high and capacity stays low, “breaking faster” is not a mystery—it’s a predictable outcome of the math.
Stress physiology evolved to be flexible. When resources are plentiful and the environment feels predictable enough, systems can afford nuance: more patience, more social bandwidth, more tolerance for ambiguity.
When energy is limited or threat has been frequent, the system becomes more conservative. It increases sensitivity—because missing danger costs more than false alarms in a depleted state. This is one reason thresholds fluctuate: your body is continuously estimating what it can afford, not what you “should” be able to handle. [Ref-3]
That estimation is not purely conscious. It’s built from sleep debt, prior strain, inflammation, pain signals, recent conflict, and the simple absence of “done” signals. In that context, faster overwhelm can be an adaptation: a way of forcing a stop when gentle signals didn’t lead to closure.
When a threshold is crossed, the nervous system often chooses speed over precision. The goal becomes immediate pressure reduction—reducing input, reducing demand, and creating distance from what feels unmanageable.
This can show up as a rapid discharge (snapping, crying, agitation) or as protection through narrowing (withdrawing, going blank, shutting down). These are not “random moods.” They are state shifts that help the body conserve resources and re-establish a sense of control or safety in the fastest available way. [Ref-4]
What if the reaction is less about the moment—and more about the system trying to stand down?
Many people interpret a low threshold as a personal flaw: “I’m too sensitive,” “I can’t handle anything,” “Other people can cope.” But the more accurate frame is capacity variability. Stress responses scale with context, physiology, and cumulative load.
A person can be deeply capable and still have a day when their system can’t keep buffering. That’s not a moral failing; it’s a sign that the internal margin has been used up. When the body is already spending resources on adaptation, there is less left for patience, flexibility, and social grace. [Ref-5]
Capacity isn’t character. It’s a condition.
Threshold problems often become self-perpetuating, not because someone “avoids feelings,” but because early signals get structurally bypassed. Modern life rewards continuation: keep going, keep responding, keep producing, keep appearing steady.
When early strain cues don’t lead to completion or relief, the system learns that subtle signals won’t change anything. It stops spending energy on gentle messaging and saves its strongest signals for when it must force an interruption. Over time, you get a loop: muted early warnings → ongoing load → abrupt breach → recovery that isn’t fully completing → lowered future threshold. [Ref-6]
In this loop, “avoidance” can look like staying functional past your real limit—not out of fear, but because there’s no clear, supported way to close the open loops you’re carrying.
When capacity is reduced, the system’s responses can look inconsistent from the outside. Internally, they often track exhaustion and overload rather than the immediate situation. [Ref-7]
These aren’t identities. They’re regulatory strategies under strain—ways the body reduces complexity when complexity is exceeding capacity.
One of the hardest consequences of a shifting threshold is not the stress itself—it’s the unpredictability. If you don’t know which version of you will show up, planning feels risky. Conversations feel loaded. Even good opportunities can feel dangerous because they might push you over the edge.
Over time, this can chip away at confidence and self-trust: “If I can’t count on myself, how can I commit to anything?” This isn’t overthinking. It’s the nervous system trying to prevent further breaches by narrowing life into what seems controllable. [Ref-8]
Unpredictability makes the world feel louder than it is.
Threshold breaches don’t just create a rough moment; they can change the next day’s baseline. After acute overload, sleep can become lighter or more fragmented, and recovery may be incomplete. [Ref-9]
When restoration is partial, the body starts the next day already closer to the edge. That can create a frustrating pattern: you “recover” just enough to resume responsibility, but not enough for your system to actually settle. Without enough settling, the buffer doesn’t fully return—and the next breach comes sooner.
This is how people end up feeling like they are always “one thing away” from snapping: not because they are fragile, but because their baseline is repeatedly rebuilt on top of unclosed strain.
It can help to separate two different processes: state change and stability. State change is what happens when something briefly soothes, distracts, or energizes. Stability is what happens when the body receives enough completion signals to stand down and stop scanning so hard.
Thresholds tend to stabilize when load is more accurately matched to recovery and when experiences are allowed to reach a sense of “done” at the nervous-system level—not just intellectually understood. This is closely tied to interoception (the body’s ability to detect internal signals) and how body–brain pathways coordinate emotion, energy, and readiness. [Ref-10]
In other words: your system doesn’t expand its capacity because you push harder. It expands when it has evidence—through repeated completion—that it won’t have to keep carrying everything indefinitely.
Stress thresholds are not purely individual. Humans regulate in relationship. When your environment carries constant evaluation, urgency, or ambiguity, your system has to spend extra resources predicting outcomes and managing impressions.
When the people around you offer clearer expectations, steadier tone, and fewer surprise demands, the body receives safety cues that reduce background scanning. This doesn’t require perfect communication; it requires fewer “unknowns” and less pressure to perform regulation on command. [Ref-11]
Support, in this frame, is not someone fixing you. It’s the social world participating in conditions where your capacity can actually return.
When thresholds stabilize, many people notice changes that are practical and bodily, not dramatic. There’s more space between stimulus and response. Small disruptions don’t instantly demand a protective shift. Social interaction costs less.
Often, it feels like signals can rise and fall without taking over. The system can mobilize and then come back down—more like a wave than a cliff. In polyvagal terms, there is greater access to states associated with safety and connection, which supports steadier engagement and faster return to baseline after stress. [Ref-12]
A stable threshold doesn’t mean life is calm. It means you’re less governed by the fear of crossing your own edge. With more predictable capacity, you can engage more intentionally—because your system isn’t constantly budgeting for an emergency.
This is where meaning becomes more available: values can guide decisions more reliably than pressure or short-term relief. Not because you “try harder,” but because the internal environment is coherent enough to hold a direction.
And because stress is buffered socially as well as biologically, steadier connection can further protect thresholds—reducing the cost of challenge and expanding what feels possible. [Ref-13]
When the edge stops moving so wildly, you can choose with more confidence.
If you’ve been “breaking faster,” it may help to treat it as data about load, closure, and capacity—not proof that something is wrong with you. The nervous system uses thresholds to prevent deeper depletion. In that sense, the break is often a boundary your body had been signaling for a while, just in quieter ways.
There is also a relational layer: isolation and disconnection can raise the cost of coping, while belonging can lower it. When support is thin, the same stressors hit harder. [Ref-14]
Respecting capacity is not shrinking your life. It’s allowing your life to become more coherent—so effort isn’t constantly spent on holding yourself together.
Understanding stress thresholds can reduce shame: the fluctuation isn’t a character glitch, it’s a living system responding to conditions. When limits are recognized and protected, the body gets the completion signals it needs to settle, and the future becomes more navigable.
Over time, this tends to support a kinder internal stance—less self-criticism for having a limit, more dignity about what your system has been carrying. That shift alone can reduce load, because compassion costs less than constant self-surveillance. [Ref-15]
And when the threshold steadies, it becomes easier to live from values instead of bracing—less governed by the next snap, more oriented toward what matters.
From theory to practice — meaning forms when insight meets action.
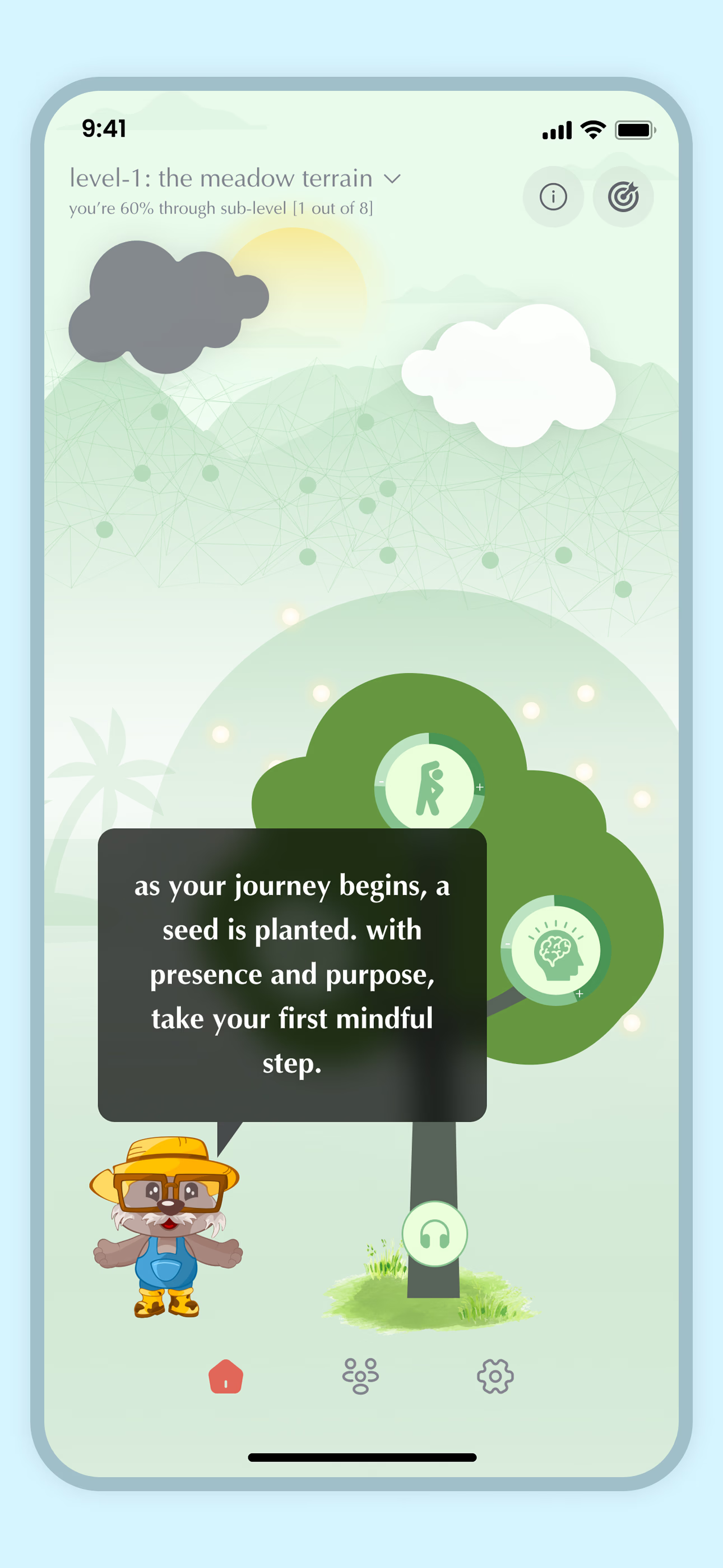
From Science to Art.
Understanding explains what is happening. Art allows you to feel it—without fixing, judging, or naming. Pause here. Let the images work quietly. Sometimes meaning settles before words do.