
Fight, Flight, Freeze: Understanding Shutdown Mode

Nervous system apps are a growing category of digital tools designed to guide body-based sequences—often breath pacing, heart-rate variability (HRV) biofeedback, short somatic routines, soundscapes, or downshift prompts. Their promise is simple: reduce physiological stress load and help the system return to a steadier baseline.
For many people, the appeal isn’t “self-improvement.” It’s the relief of structured guidance when the body is stuck in urgency, tension, or blankness—when thinking harder doesn’t help, and the day keeps moving anyway.
What if the point isn’t to become calmer as a personality—but to give your system more reliable “stand-down” signals?
Chronic stress doesn’t always feel dramatic. Often it looks like shoulders that won’t drop, a jaw that stays braced, sleep that never quite repairs, or a mind that keeps scanning for what’s next. These patterns aren’t character flaws; they’re the nervous system staying online because it hasn’t received enough cues that a cycle has completed.
When load is high, self-generated calming can be hard to access. Not because someone is doing it wrong, but because the body is using its energy to maintain readiness. In that state, external structure—timing, pacing, a guided sequence—can feel like borrowing a rail when balance is limited.
Research on brief app-based biofeedback suggests that even short guided interventions can improve stress recovery after a stressor, which fits with this “borrowed structure” idea: the app supplies a pattern the body can follow when it’s over-activated. [Ref-1]
Most regulation apps work by shaping rhythm and attention in ways that influence autonomic function: heart rate patterns, breathing rate, and the balance between mobilization and rest. HRV biofeedback, for example, uses paced breathing and feedback signals to help the body practice a more flexible cardiac rhythm—often associated with better stress tolerance and recovery. [Ref-2]
This isn’t about “positive thinking.” It’s closer to tuning. When breathing slows and becomes more coherent, vagal pathways can support a downshift in threat physiology—less bracing, less internal acceleration, more capacity for signals to return. Over time, that repeated downshift can make it easier for the system to find a calmer range after activation.
In other words: the sequence isn’t trying to convince you that you’re safe; it’s giving your body a pattern that sometimes allows safety physiology to appear.
Autonomic systems are built for variability: activation when something needs responding to, then completion and settling afterward. In many modern lives, the “afterward” keeps getting interrupted—by constant messaging, ongoing evaluation, open loops, and the sense that nothing is ever fully done.
In that mismatch, states like anxiety, avoidance, craving, and overcontrol can be understood as regulatory responses to incomplete closure. They keep the system moving when completion signals are scarce, or they reduce exposure to demands when load is already too high. A meta-analysis of HRV biofeedback training has found meaningful reductions in stress and anxiety, consistent with the idea that training autonomic flexibility matters when modern stress becomes prolonged. [Ref-3]
When threat becomes a background condition, the body can start treating “ordinary life” like the part where it still has to stay ready.
Many people report that a guided breath pace, a vibration cue, or a simple biofeedback display can shift their state within minutes. That quick effect is often the nervous system responding to clear, repetitive cues: predictable rhythm, reduced uncertainty, and a narrow focus that temporarily quiets competing demands.
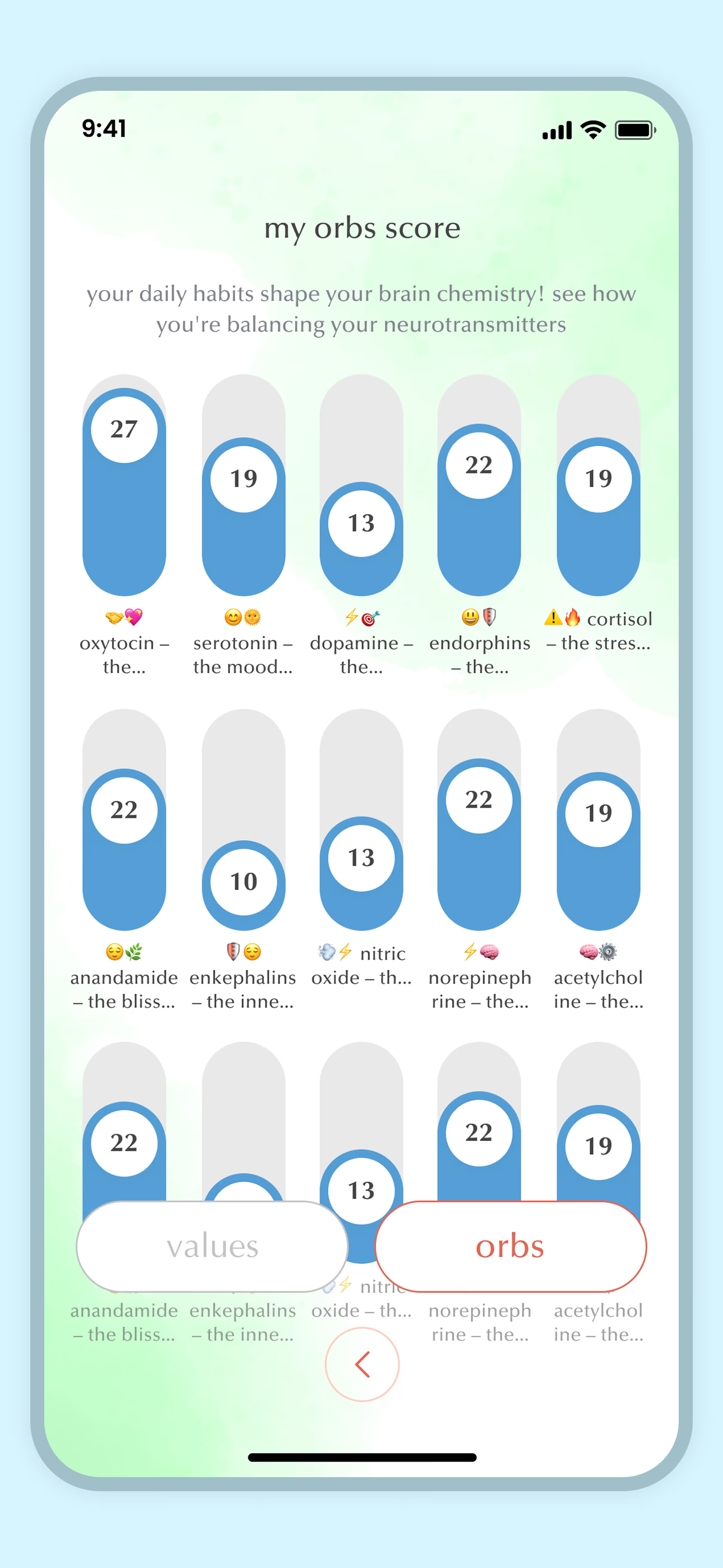
Some app designs add “gameful” elements—visuals, scoring, progress indicators—which can strengthen engagement while the body is learning the rhythm. Studies of breathing training apps have shown increases in HRV and self-reported relaxation after paced-breathing sessions, supporting the plausibility of rapid, measurable downshifts. [Ref-4]
It’s important to name what this is and isn’t. This is state change—physiological calming—often very real and very helpful. It is not automatically the same thing as the deeper settling that comes when life experiences reach completion.
It’s easy to assume that if something produces calm, it must be “fixing” the system. But regulation tools are more like stabilizers than permanent rewiring on their own. They can lower arousal, create a pause, and reduce perceived threat long enough for the body to regain capacity.
Research on brief smartphone-based mindful breathing tasks shows that even short, app-delivered protocols can influence HRV and stress-related outcomes. [Ref-5] That supports a practical reality: repetition matters. A single downshift can help. Repeated downshifts can train familiarity with the pathway.
Still, lasting stability usually requires more than repeated calming. The nervous system tends to settle most durably when important loops actually complete—when there is an “it happened, it’s handled, it’s integrated into life” signal, not just a temporary reduction in activation.
One way to understand these tools is as scaffolding: they can reduce immediate physiological load so a person has more room to orient—toward relationships, responsibilities, values, and the parts of life that need finishing. When arousal decreases, attention becomes less dominated by urgency, and the system can sometimes track what actually matters.
HRV biofeedback is often described as a low-risk method that can support vagal tone and autonomic flexibility, which can translate into a steadier platform for everyday functioning. [Ref-6] That steadier platform can make it more possible for experiences to reach closure—through conversation, decisions, boundaries, grief completion, repair, or simply the felt sense of “done.”
The key distinction: an app can support regulation; completion supports integration. They can work together, but they are not interchangeable.
When guided regulation is a good fit, the changes are often subtle but meaningful: not a new personality, but more recovery capacity. Methods literature on HRV biofeedback describes common protocols (like resonance breathing) and links them to autonomic regulation—suggesting why certain effects show up consistently across users. [Ref-7]
None of this requires moralizing. It’s not “doing better.” It’s the system having more reliable return paths after activation.
There’s a predictable risk with any external regulator: the body can start treating the tool as the primary cue for settling. In that pattern, calm may feel accessible only when the app is open, the timer is running, or the feedback graph is visible.
This doesn’t mean someone is dependent in a personal-failure sense. It can simply mean the environment still doesn’t provide enough natural closure, so the nervous system prefers the most reliable cue available. Research showing that even a single HRV biofeedback session can improve attentional control under stress highlights how quickly the system can “lock onto” a guided signal. [Ref-8]
When this happens, the issue isn’t a lack of insight. It’s a structural imbalance: lots of activation and evaluation, not enough completion. The app becomes a bridge—but the bridge can’t replace arriving.
Many apps lean on reminders, streaks, scheduled prompts, and short protocols. While those features can feel simplistic, they address a real nervous-system problem: under load, initiation is costly. A prompt reduces the cost of starting; a structured sequence reduces the cost of deciding what to do; feedback reduces the ambiguity of whether anything changed.
Mobile HRV biofeedback research discusses how everyday implementation can support emotional regulation outside the clinic, partly because the device makes practice easier to repeat in real contexts. [Ref-9] Over time, repetition can create a more familiar pathway for recovery—less like “calming down” and more like returning to a known range.
Structure isn’t motivation. It’s friction reduction for a system that’s already spending energy managing unfinished demands.
When practice is consistent over time, many people notice something beyond momentary relief: the nervous system becomes less rigid. Activation still occurs—because life still happens—but the return is smoother. This is often described as improved autonomic flexibility: the ability to mobilize when needed and settle when the moment is complete.
Breathing-based interventions have been associated with improvements in HRV, perceived stress, and attention-related outcomes, which helps explain why some people feel more stable even outside the practice window. [Ref-10] Importantly, that stability isn’t “better thoughts.” It’s a system that can allocate attention more freely because it isn’t spending as much bandwidth on background threat monitoring.
This is a meaning bridge, too: when the body is less preoccupied with internal alarm, it becomes easier to sense what fits, what matters, and what needs completion for life to feel coherent.
Nervous systems don’t regulate in isolation. Co-regulation—settling in the presence of a steady other—has always been part of human threat and safety physiology. That’s why coaching, peer-guided sessions, or group formats can change the experience of a tool from “something I do to myself” to “something that happens with support.”
Some apps explicitly include coaching or community layers (for example, tools that combine somatic exercises, breathing, tracking, and guided support). [Ref-11] The science-friendly interpretation here is not that other people “fix” you—it’s that social safety cues can reduce baseline vigilance, which makes practice more available and less effortful.
Sometimes the most regulating signal isn’t the technique. It’s the sense that you don’t have to hold everything alone.
People often imagine regulation as feeling relaxed all the time. In practice, steadier regulation is usually more practical than that: fewer spikes, less internal urgency, and more accurate readouts from the body. The goal isn’t constant softness—it’s reliable recovery and clearer signals.
Breathwork apps popularize different protocols for calm, focus, and sleep, which maps onto the idea that regulation involves shifting states appropriately rather than staying in one state. [Ref-12] When capacity returns, signals can come back online: hunger is hunger, fatigue is fatigue, “no” feels clearer, and rest can actually register as rest.
Over time, some users notice a shift: they don’t need the full guided sequence to access the pathway. The breath pace becomes familiar. The body recognizes the rhythm sooner. A short pause, a few cycles, or a remembered cue can be enough to begin returning.
This is where autonomy starts to emerge—not as self-control, but as learned access. Apps that guide resonance breathing make this transfer easier because the rhythm is simple and repeatable, even without the screen. [Ref-13] The app was the training wheels; the nervous system keeps the pattern.
And importantly, this is also where meaning can re-enter: as the system stabilizes, experiences can complete. Life stops feeling like a set of tabs left open, and begins to feel more inhabitable.
Nervous system apps are often at their best as scaffolds: they provide rhythm, structure, and feedback when stress load is high and internal cues are hard to access. They can reduce activation enough for the day to become workable again, and they can help practice a return pathway so recovery is less random.
But they are not substitutes for completion. An app can change state; it can’t, by itself, finish the unfinished parts of life—the conversations that need repair, the boundaries that create safety, the grief that needs a “done” signal, the identity-level coherence that comes from living in alignment over time.
In a digital wellness landscape filled with somatic and breath-based options, it can help to hold a respectful frame: tools can support the body without becoming the place where life gets resolved. [Ref-14]
Sustainable regulation usually isn’t a breakthrough. It’s a gradual increase in the system’s ability to return—again and again—until “coming back” becomes more familiar than staying braced. Technology can support that training, including biofeedback and even more immersive formats that enhance stress management effects. [Ref-15]
And when the body has more reliable stand-down signals, meaning tends to get denser: choices feel less frantic, attention is less fragmented, and identity can settle around what is actually lived—especially when experiences are allowed to complete.
That’s not self-optimization. It’s the nervous system learning it can finish a loop, and that life can feel coherent again.
From theory to practice — meaning forms when insight meets action.
From Science to Art.
Understanding explains what is happening. Art allows you to feel it—without fixing, judging, or naming. Pause here. Let the images work quietly. Sometimes meaning settles before words do.