Mind-Body Loops: How Emotional Stress Shows Up Physically

Sometimes the hardest mental health days aren’t dramatic. They’re flat, foggy, and strangely effortful—like your mind is moving through thick air. You can still show up, still function, and still feel inexplicably off.
One under-discussed reason is chronic, low-grade inflammation: a long-running immune “on” signal that can change how the brain manages mood, focus, and threat detection. This isn’t about weakness or attitude. It’s about load.
What if your mood isn’t just a story in your head—but a state your body is holding?
Inflammation-linked mental disruption often shows up as a mismatch: the outside looks manageable, but the inside feels strained. Small tasks feel heavy. Minor stressors land like major ones. Your patience shortens, your thinking slows, and your emotional steadiness feels less available.
This can be especially confusing because it doesn’t always map neatly onto current circumstances. The mind searches for explanations—work, relationships, personality—while the body may be running a quieter, biological alarm that changes the whole tone of experience. [Ref-1]
It can feel like you’re reacting to life through a fogged-up window: the scene hasn’t changed, but your access to it has.
The immune system doesn’t only fight infections. It also communicates with the brain through signaling molecules (including cytokines) that influence how the nervous system allocates attention, energy, and vigilance. When this signaling becomes persistent, the brain may shift toward scanning for problems and conserving resources. [Ref-2]
In practical terms, chronic inflammatory signaling can intersect with neurotransmitter systems, stress-hormone dynamics, and brain circuits involved in motivation and emotion regulation. The result can resemble “psychological” symptoms—low mood, irritability, anxiety, reduced pleasure, slowed thinking—without those symptoms being purely psychological in origin.
Inflammation is not a mistake. It’s a protective response built for short bursts: detect a threat (like injury or infection), mobilize resources, repair, then stand down. In that short-term context, it’s coherent: it helps you survive and recover.
The modern problem is not inflammation itself—it’s duration. Many present-day conditions can keep the immune system in a low-grade activated state for long stretches, even when there is no clear “fight” to finish. When the body doesn’t get a clean completion signal, defense becomes a background setting rather than a brief phase. [Ref-3]
When inflammation stays elevated, the body often behaves as if it needs to conserve energy and reduce exposure. This can look like fatigue, reduced drive, less cognitive flexibility, and a narrower emotional range—not because something is “wrong with you,” but because the system is prioritizing protection over exploration. [Ref-4]
From a meaning-and-coherence perspective, this matters: creativity, social warmth, and future planning are resource-intensive. When the body is allocating resources toward defense and repair, the mind may have less capacity to generate a felt sense of “enough,” “done,” or “safe.” That unfinished feeling can keep the system tense, even on quiet days.
Many people learn to interpret mood changes as evidence about their character, mindset, or coping skills. That lens can accidentally add pressure: if you feel low, you’re supposed to think differently; if you feel anxious, you’re supposed to calm down; if you feel numb, you’re supposed to “open up.”
But inflammation blurs the boundary between “mental” and “physical.” Immune dysregulation can directly influence mood and anxiety patterns, meaning your experience may be shaped by physiology even when you’re doing everything “right.” Seeing this clearly doesn’t create instant relief—but it can reduce shame and restore orientation: something real is happening in the system. [Ref-5]
What changes when you treat your mood as a signal of load, not a verdict?
In a chronically inflamed state, the nervous system has fewer spare resources. Engagement costs more. Social contact can feel noisy. Movement can feel like too much. This often leads to a quiet pattern of pulling back—not as a psychological choice, but as a load-based reduction in output.
Here’s where the loop forms: withdrawal can reduce immediate strain, yet it can also reduce the very inputs that help the body stand down—rhythm, nourishment cues, restorative sleep pressure, and stabilizing connection. Over time, “less engagement” and “less recovery” can coexist, sustaining inflammatory load in everyday life. [Ref-6]
Because inflammation affects energy allocation and brain signaling, it can express as familiar mental patterns. These aren’t identities. They’re nervous-system strategies under strain.
When these show up together, it can help to hold a wider frame: the system may be working to protect itself while lacking the conditions to fully complete the cycle. [Ref-7]
Resilience isn’t a personality trait. It’s a capacity state: how quickly your system can return to baseline after demand. Chronic inflammation can reduce that return speed. The result is not simply “feeling worse”—it’s reduced room to absorb life without tipping into irritability, worry, or shutdown. [Ref-8]
Motivation also becomes less reliable when the body is in sustained defense. It’s harder to access the internal “yes” that makes engagement feel coherent. Without that felt coherence, the mind may default to short-term stabilizers—avoidance, numbing, overcontrol—not because you’re choosing dysfunction, but because the system is seeking a manageable state.
Inflammation-driven fatigue can reduce movement, disrupt sleep architecture, and shrink stress tolerance. Each of those shifts can, in turn, keep immune signaling elevated. This isn’t a moral spiral; it’s a structural one—inputs and outputs stop matching the body’s need for closure. [Ref-9]
In this loop, “rest” can become complicated: you may be exhausted yet not restored, tired yet wired, or sleepy yet unrefreshed. The nervous system remains partially mobilized, and the brain interprets that mobilization as a reason to stay vigilant—further amplifying anxious or low mood states.
When inflammatory signaling begins to reduce, many people describe a gradual internal shift: thoughts feel less sticky, mood swings soften, and attention becomes more available. This change often isn’t dramatic. It can feel like the system is finally getting the message that it can stand down. [Ref-10]
Importantly, this kind of stabilization is not the same as insight or reframing. You can understand your patterns perfectly and still feel dysregulated if the body is carrying defense-level load. When the load decreases, the return of clarity can feel physical: a quieter baseline, more consistent energy, and fewer false alarms.
It’s less like “I figured it out,” and more like “my system stopped bracing.”
Chronic inflammation can make social life feel effortful: conversation takes more energy, conflict feels sharper, and small misunderstandings can land with surprising intensity. In that state, irritability isn’t a character flaw—it’s often a sign that the system has little buffer.
As internal regulation improves, many people notice they can stay present longer, recover faster after tension, and offer more availability without forcing it. The tone of interaction changes because the baseline state changes—less defensive load means more room for connection signals to register. [Ref-11]
When the body isn’t continuously sending immune distress signals, the brain can reallocate resources toward planning, nuance, and flexible attention. That can look like improved concentration, steadier mood, and more reliable stress tolerance—not as a performance upgrade, but as a return to a more sustainable operating mode. [Ref-12]
This is also where emotional range tends to normalize: not “more intense feelings,” but more accurate ones. The system can distinguish between real problems and background noise, allowing signals to rise and fall instead of staying stuck at high volume.
When chronic inflammation eases, agency often returns in a specific way: you’re less busy managing symptoms and more able to orient toward what matters. Values become practical again—because they’re no longer competing with constant internal depletion.
Meaning, in this sense, isn’t motivational hype. It’s what emerges when life experiences can complete and settle into identity—when the nervous system has enough stability to register closure and enough energy to participate in the world. Chronic inflammation disrupts that across the lifespan by keeping the body in partial defense. [Ref-13]
What matters to you can feel clearer when your body isn’t spending all day protecting you.
If your mood has felt unreliable, your motivation thin, or your mind persistently foggy, it can help to consider a body-based lens. Inflammation-related shifts can be real drivers of anxiety and depression-like experiences, not just reactions to life events or internal narratives. [Ref-14]
This framing doesn’t erase the complexity of mental health, and it doesn’t reduce a person to biology. It simply returns dignity to the experience: your system may be responding to sustained load and incomplete recovery. When the conditions for restoration return, the mind often follows—not through willpower, but through physiology finding its way back to “safe enough.”
Many people spend years trying to think their way into steadiness. Sometimes the missing piece is not effort or insight, but a body that hasn’t been given a true “done” signal.
As inflammation quiets, emotional clarity often returns as a natural consequence: the brain becomes less threat-shaped, attention becomes more coherent, and engagement feels possible again. Not because you forced it—because the conditions for stability came back online. [Ref-15]
From theory to practice — meaning forms when insight meets action.
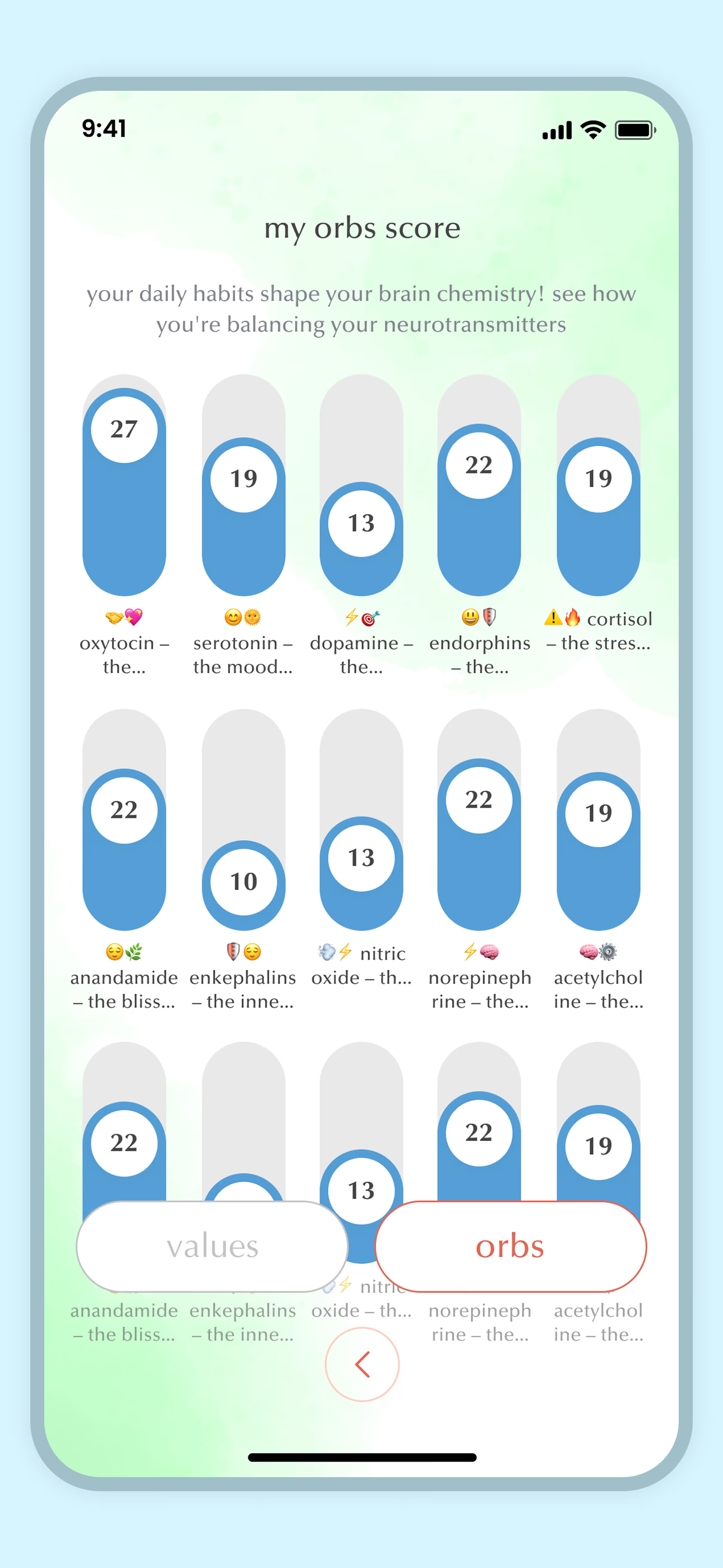
From Science to Art.
Understanding explains what is happening. Art allows you to feel it—without fixing, judging, or naming. Pause here. Let the images work quietly. Sometimes meaning settles before words do.